Treatments for localized prostate cancer
Localized prostate cancer (at stages T1 and T2) can be treated using a variety of methods, depending on the characteristics of the disease and the patient’s preferences.
Active Surveillance
When prostate cancer is localized with low risk of evolution, an active surveillance strategy can be proposed. This therapeutic option consists in a regular clinical exam to check the cancer expansion: PSA monitoring, prostate biopsies and/or regular MRI. In case of expansion, a prostate cancer treatment strategy will be suggested to the patient.
Major advantage of this therapeutic approach is to avoid or delay side effects of prostate cancer treatments. A disadvantage for this approach are the repeat biospies: even if it is a minimally invasive treatment, it is still a surgery with possible side effects. Another disadvantage of this approach is the psychological point on patients that can be anxious with this active surveillance.
HIFU (High Intensity Focused Ultrasound): the non-invasive treatment, incisionless and radiation free

HIFU treatment involves destroying cancerous cells in the prostate and so prostate cancer by destroying with focused ultrasound. A probe is inserted into the patient’s rectum under spinal or general anesthesia. The probe can both visualize the prostate and generate focused ultrasound. Treatment can be total (whole prostate is treated), partial (part of the prostate is treated) or focal (only the prostate area affected by the cancer is treated). For focal treatment, the physician will determine the area to be destroyed thanks to the elastic fusion of the diagnostic images (MRI or biopsy) with the real-time ultrasound images allowed by the probe.
HIFU treatment lasts between 1:30 and 2:30 and can be performed on an outpatient basis or with a short hospital stay (1 or 2 nights). Being a non-invasive technique preserves patient’s quality of life by decreasing the side effects associated with conventional radical treatments (incontinence and erectile dysfunction).
HIFU treatment may have some side effects. If the risks of incontinence and erectile dysfunction are low, they can happen.
Radical prostatectomy – surgery
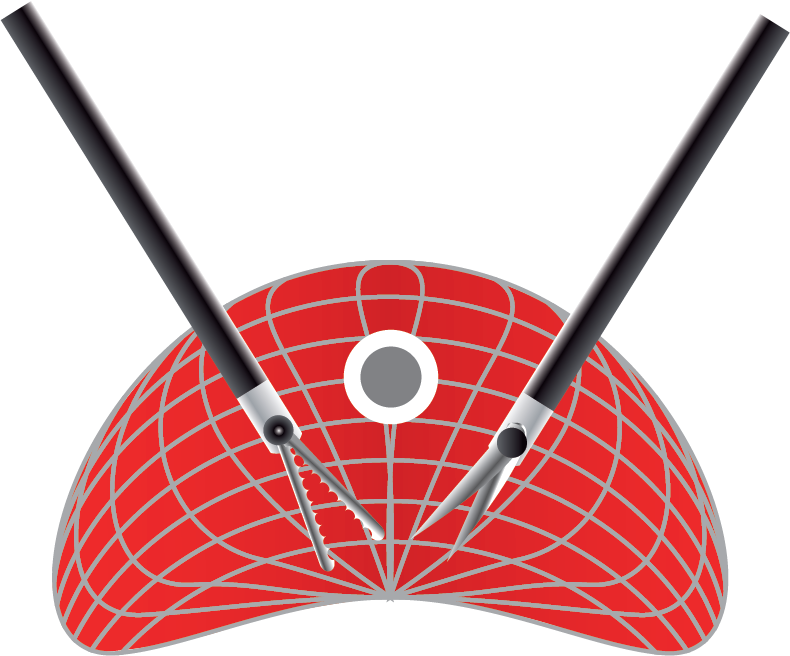
Radical prostatectomy (or total prostatectomy) involves surgically removing of the prostate and seminal vesicles. It is a major surgery under general anesthesia performed by an incision under the umbilicus (open surgery) or through small incisions allowing insertion of tools for the surgery (coelioscopic surgery and/or robotic assisted). After removal of the entire prostate and seminal vesicles, the bladder is binded to the urethra by a suture.
Hospitalization time varies between 5 and 7 days, sometimes more.
The radical prostatectomy survival rate is superior to other therapeutic options since it guarantees the eradication of cancer localized into the prostate. Post-operative cell analysis may determine if the cancer has spread out of the capsule. Recovery and return to a normal life depend on the patient physical condition before treatment and to its ability to recover after treatment. It takes at least about 3 to 4 weeks to recover.
In the long run, main side effects are sexual disorders (inability to have or maintain an erection) and incontinence (inability to retain urine; this is temporary and it progressively declines).
With a short term, rare but possible complications inherent to the intervention are:
- Haemorrhage
- Urinary tract infection
- Rectal wound
- Hematoma
External radiotherapy – X-ray treatment

The patient is subjected to high-dose rays directed at the prostate. These rays destroy the cells by causing lesions in their DNA.
The treatment is divided into approximately 40 sessions over a period of 6 to 8 weeks. During each session, which lasts around 20 minutes, the patient remains immobile on the treatment table while the machine is delivering the rays. The treatment is painless.
External radiotherapy avoids general anesthesia and surgery with potential complications. The major disadvantage is the impossibility to do surgery in case of failure of radiotherapy.
Erectile dysfunction may occurs in the long run (inability to have or maintain an erection). With a short term, possible complications are:
- Skin irritation
- Fatigue
- Bladder irritation
- Digestive disorders
- Diarrhoea, bloody stool
Curietherapy, radium therapy or brachytherapy – radioactive implants
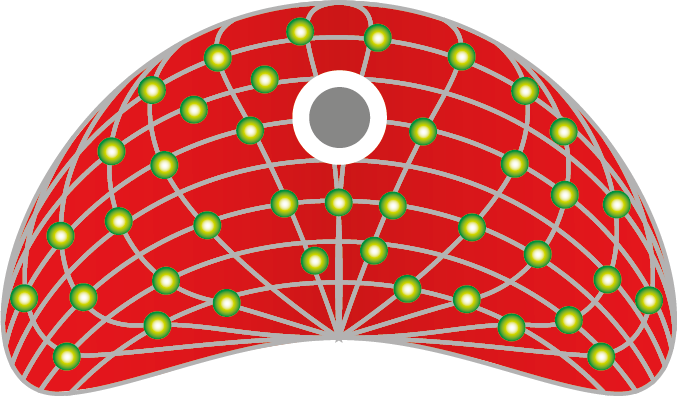
Radium therapy, also known as brachytherapy, involves temporarily or permanently implanting between 50 and 100 tiny seeds of radioactive material into the affected area. These seeds constantly emit rays that destroy prostate cells by causing lesions in their DNA. This procedure is performed under general anesthesia. After a urinary tract catheter installation, an endorectal probe is introduced into the rectum to visualize the prostate and realize in real time planning and dosimetry in 3D. When implanting the seeds, the surgeon is guided by an ultrasound scanner (with a probe inserted into the patient’s rectum). Then the seeds act by radioactive emission over a few millimeters.
Hospitalization delay is often 2 days but it can vary depending on planned treatment type. A rectal preparation (enema) may be necessary before surgery.
This technique advantage is the fact that the highest dose is delivered where it is necessary, restricting this dose to next organs. It reduces associated side effects. Even if radioactivity is reduced with time and distance, patient has to respect some precautions during the first treatment weeks. Immediate side effects are a hematoma to the perineum (needles insertion zone), bloody urine and fatigue. Later, patients may notice erectile dysfunction and/or a less quantity of sperm or even urinary disorders.
Cryotherapy – cold-based treatment
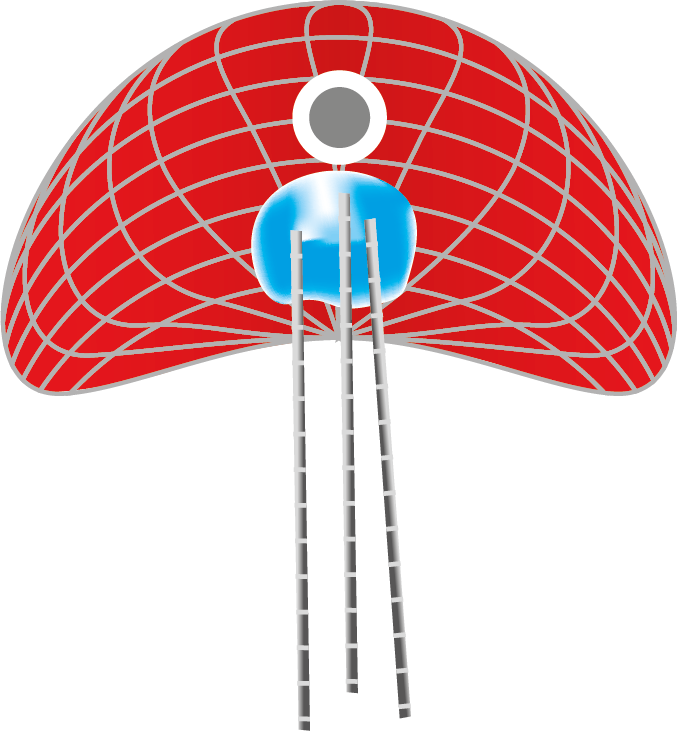
Cryotherapy is a technique that freezes the prostate by inserting needles generating temperatures below 0°C. Operation is performed under spinal or general anesthesia. An endo-rectal ultrasound probe locates the prostate and allows the volume to be evaluated. The needles intended to deliver the cold will then be placed according to a precise cartography through the perineum. A urethral catheter is placed into the bladder to protect the urethra and urinary sphincter from cold-induced injury.
Hospitalization delay is about 48 hours.
Cryotherapy destroys tissues but preserves protein frame which supports cicatrisation. However, it is important to accurately identify the size and volume of the area to be treated and to calculate the needed margins. If tumor cells remain surrounding the frozen zone, these cells have the ideal environment to proliferate.
The main complication is still erectile dysfunction (inability to have or maintain an erection).
Treatments for advanced prostate cancer
Hormone therapy
Hormone therapy blocks testosterone action (steroid hormones) on cancer cells to stop the cancer progression. It also reduces pain or symptoms related to the cancer (palliative treatment).
The drugs are most often given orally, injected under the skin or intramuscularly.
When cancer is advanced, hormone therapy is an effective way to control cancer. It also contributes to reduce some cancer symptoms like urinary symptoms and pain related to the metastases. It can be used in combination with other treatments to make those more effective. The main hormone therapy disadvantage is that it can slow cancer growth but cannot cure it. Furthermore, its effects are of limited duration that varies from one patient to another.
Undesirable effects related to treatment are:
- Hot flush
- Erectile dysfonction
- Reduced libido
- Weight gain
- Reduction in bone mass
- Chest puffiness and sensitivity
- Irritability
Chemotherapy
Chemotherapy is used to treat patients who have resistance to hormones. This treatment decreases tumor growth and can decreases pain related to cancer. The patient takes drugs that destroys cancer cells and prevents it from growing.
The majority of drugs used are administered intravenously, or orally. Sessions can take place in standard hospitalization, in hospital day care or at home. Sessions frequency and treatment delays depend on cancer.
Chemotherapy is an effective treatment that can be used alone or in combination with other treatments (surgery or radiotherapy…). By destroying cancer cells, chemotherapy also attacks healthy cells and affects the entire patient’s immune system.
Most common and known side effects are:
- Blood count modification (decrease of some white blood cells, red blood cells and blood platelets)
- Digestive disorders (nausea, vomiting, diarrhoea, constipation…)
- Hair loss
- Fatigue
Radiotherapy – X-ray treatment
In patients with metastatic cancer, radiotherapy can soothe the disease’s symptoms and contains the disease from spreading.
